Overview
A kidney transplant is the transfer of a healthy kidney from one person into the body of a person who has little or no kidney function.
The main role of the kidneys is to filter waste products from the blood and convert them to urine. If the kidneys lose this ability, waste products can build up, which is potentially life-threatening.
Loss of kidney function, known as end stage chronic kidney disease or kidney failure, is the most common reason for needing a kidney transplant.
Other treatment options for end-stage chronic kidney disease include dialysis.
Who can have a kidney transplant?
Most people who need a kidney transplant are able to have one, regardless of their age, as long as:
- they're well enough to withstand the effects of surgery
- the transplant has a relatively good chance of success
- the person is willing to comply with the recommended treatments required after the transplant – such as taking immunosuppressant medication and attending regular follow-up appointments
Reasons why it may not be safe or effective to perform a transplant include having an ongoing infection (this will need to be treated first), severe heart disease, cancer that has spread to several places in your body or AIDS.
Kidney donations
Unlike many other types of organ donation, it's possible to donate a kidney while you are alive because you only need 1 kidney to survive. This is known as a living donation.
People who want to be considered as a kidney donor are tested very carefully to ensure they are a suitable donor and are fit for the operation needed to remove a kidney.
Ideally, living donations will come from a close relative because they are more likely to share the same tissue type and blood group as the recipient, which reduces the risk of the body rejecting the kidney.
Kidney donations are also possible from people who have recently died. This is known as deceased kidney donation. However, this type of kidney donation has a slightly lower chance of long-term success.
Find out more about kidney donation on the NHS Blood and Transplant website
Waiting for a kidney
People who need a kidney transplant, but do not have a suitable living donor, will have to wait until a suitable deceased donor kidney becomes available.
On average, the waiting time for a deceased donor kidney transplant is 2 and a half to 3 years. Waiting times are so long because the demand for donated kidneys in the UK is far higher than the available supply of donors.
Kidney donors are particularly required from people of non-white ethnic origin, because rates of kidney disease are especially high in people of South Asian, African and Caribbean ethnic origin. However there are not many donors from these communities.
The transplant procedure
If you receive a kidney from a living donor, this will be a carefully planned operation.
If you are waiting for a deceased donor kidney, the transplant centre will contact you if a suitable kidney becomes available. This can happen at any time of the day or night. Staff at the centre will check you do not have any new medical problems and will ask you to go to the centre, where final checks will be performed to be sure the transplant should go ahead.
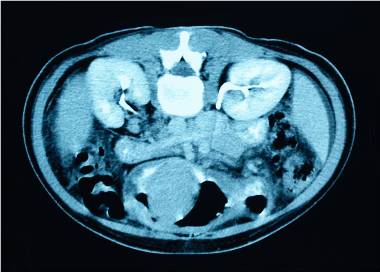
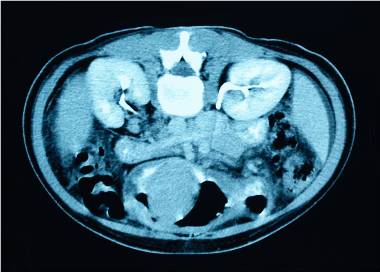
You'll then have surgery to insert the new kidney and connect it to your blood vessels and bladder. The new kidney will be placed in the lower part of your abdomen (tummy). Your own kidneys will usually be left in place.
A kidney transplant is a major surgical procedure with a wide range of potential risks. In the short term, these risks include blood clots and infection. Longer term problems, which include diabetes and an increased risk of infections, are usually related to the medicine you need to take to reduce the chance of your body rejecting the kidney.
Because of the risk of further problems, people who have had a kidney transplant require regular check-ups for the rest of their life.
Living with a kidney transplant
Having a healthy lifestyle after a kidney transplant goes a long way to minimising the risk of complications.
Therefore, it’s recommended that you:
- stop smoking if you smoke
- eat a healthy diet
- lose weight if you are overweight or obese
- take steps to reduce your risk of developing infections
How long do kidney transplants last?
There are a number of factors which affect how long a transplanted kidney lasts.
These include whether or not the kidney came from a living donor, how well the kidney is matched in terms of blood group and tissue type, and the age and overall health of the person receiving the donation.
If you have a kidney transplant that fails, you can usually be put on the waiting list for another transplant. You may need dialysis in the meantime.
Organ donation in Wales
Wales moved to a soft opt-out system for organ donation on 1 December 2015. Under the soft opt-out system, if you have not registered a clear organ donation decision (opt-in or opt-out), you will be treated as having no objection to being an organ donor. This is called 'deemed consent'.
It is called a soft opt-out system because your family will always be involved in all discussions about donation. They will need to be present to answer questions about your health, lifestyle and where you lived. They could also say if you knew you did not want to be an organ donor. To learn more about organ donation in Wales click here.
Waiting list
Ideally, a kidney transplant should be performed when tests show that the extent of damage to your kidneys is so great that you will require dialysis within the next 6 months.
However, because of the lack of available kidneys, it's unlikely you will receive a kidney donation at this time, unless a family member or friend who has a similar tissue type is willing to make a living donation.
Find out more about living donations on the NHS Blood and Transplant website.
Most people with kidney failure need dialysis while they wait for a donated kidney to become available.
The average time a person spends on the waiting list for a kidney transplant is 2 to 3 years, although it can be shorter or longer than this.
How donations are allocated
Demand for donations from recently deceased people far outstrips supply so there are strict but necessary guidelines about how donations are allocated.
Children and young adults are generally given priority if a matched donation becomes available, as they'll most likely gain a longer-term benefit from a donation.
For older adults, a scoring system is used to determine who should get a donation. The score is based on factors such as how long you've been on the waiting list and how well matched the donor is in terms of tissue type, blood group and age.
You may have a longer wait for a kidney if you have high levels of antibodies in your blood that might make it harder for you to receive a transplant. This is called desensitisation and can happen after a blood transfusion, pregnancy or previous transplant.
Waiting for a transplant
If you're on the waiting list for a kidney, the transplant centre will need to contact you at short notice once a kidney becomes available, so you must inform staff if there are any changes to your contact details.
You should also inform staff if there are changes to your health – for example, if you develop an infection.
While waiting for a donated kidney to become available, it is important you stay as healthy as possible by:
Make sure you always have an overnight bag ready for when the call comes and make arrangements with friends, family and work so you can go to the transplant centre as soon as a donor kidney becomes available.
Transplant centres
Find out more about kidney transplant units on the NHS Blood and Transplant website
How is it performed?
When a suitable donor kidney is found, the transplant centre will contact you. Staff at the centre will check you don't have any new medical problems and will ask you to go to the centre.
When you hear from the transplant centre:
- do not eat or drink anything
- take all current medicines with you
- take a bag of clothes and essential items for your hospital stay
When you arrive at the transplant centre, you'll be quickly assessed. Some of the tests you had at your initial assessment may be repeated to ensure no new medical conditions have developed. Tests will also be done to ensure the donor kidney is suitable for you.
The transplant procedure must be carried out as quickly as possible for the transplant to have the best chance of success. After the medical team has confirmed the kidney is in good condition and is suitable, you'll be given the general anaesthetic and taken to the operating theatre.
The operation
The kidney transplant procedure involves 3 main stages:
- First, an incision (cut) is made in your lower abdomen (tummy), through which the donated kidney is put into place. Your own kidneys will usually be left where they are, unless they're causing problems such as pain or infection.
- Second, nearby blood vessels are attached to the blood vessels of the donated kidney. This is to provide the donated kidney with the blood supply that it needs to function properly.
- Finally, the ureter (the tube that carries urine from the kidney to the bladder) of the donated kidney is connected to your bladder.
A small plastic tube called a stent may be inserted into the ureter to help ensure a good flow of urine initially. This will usually be removed about 6 to 12 weeks later during a minor procedure called a cystoscopy.
When the kidney is properly in place, the incision in your abdomen will be closed with surgical staples, stitches or surgical glue.
Although the procedure may sound relatively straightforward, it's very demanding and complex surgery that usually takes around 3 hours to complete.
After the operation
Once you have recovered from the effects of the anaesthetic, it's likely you will feel some pain at the site of the incision. Painkillers will be provided, if necessary.
After the operation, you'll immediately begin treatment with medication designed to prevent your immune system from rejecting your new kidney.
Most transplanted kidneys will start working within a week or 2. You may need to have dialysis until your transplanted kidney is working properly.
Most people can leave hospital in about a week, but you'll need to attend frequent appointments at the transplant centre so your kidney function can be assessed and tests can be carried out to check how well your medicines are working.
For the first month after surgery, you may need to have 2 to 3 appointments a week. However, over time, your appointments will become less frequent. After a year, as long as you do not have any serious problems, you should only have to attend the centre once every 3 to 6 months.
After kidney surgery, you should be able to return to work and normal activities within a few months, provided you make good progress.
Living with
The following lifestyle advice is usually recommended to help you stay healthy after a kidney transplant.
Stop smoking
If you smoke, it's strongly recommended you stop as soon as possible because smoking can reduce the life of your new kidney and can increase your risk of developing some types of cancer.
The Help Me Quit website can provide support and advice to help you stop smoking, and your GP can also recommend and prescribe treatments that can help.
Diet
Most people are able to enjoy a much more varied diet after a kidney transplant, although you may be advised to avoid some foods after the operation until the kidney is working properly.
During the early stages after a transplant, while you're on higher doses of immunosuppressant medication (see below), you should avoid eating foods that carry a high risk of food poisoning, including:
- unpasteurised cheese, milk or yoghurt
- foods containing raw eggs (such as mayonnaise)
- undercooked or raw meats, fish and shellfish
Once your kidney is working properly and the best immunosuppressant dose for you has been identified, you'll usually be advised to follow a generally healthy diet, as this can help reduce your risk of complications such as diabetes.
A healthy diet should include:
- at least 5 portions of fruit and veg a day
- plenty of potatoes, bread, rice, pasta and other starchy foods; ideally you should choose wholegrain varieties
- some milk and dairy foods
- some meat, fish, eggs, beans and pulses and other non-dairy sources of protein
Avoid food that contains high levels of salt, as salt can cause high blood pressure, which can be dangerous in people with a kidney transplant.
Exercise and weight loss
Once you've started to recover from the effects of surgery, you should try to do regular physical activity.
Adults should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity every week. This includes any activity that increases your heart and breathing rate - it may make you sweat but you are still able to hold a normal conversation.
Examples include:
- fast walking
- riding a bike on level ground or with few hills
- swimming
- tennis
Choose physical activities that you enjoy, as you're more likely to continue doing them.
It is unrealistic to meet these exercise targets immediately if you have not exercised much in the past. You should aim to start gradually and then build on it.
If you are overweight or obese you should try to achieve a healthy weight. This can be safely done through a combination of eating a healthy, calorie-controlled diet and regular exercise. Aim for a body mass index (BMI) of between 18.5 and 25.
Read more about exercise.
Alcohol, drugs and medicines
Regularly drinking alcohol above the maximum limits can raise your blood pressure, which can be dangerous for people with a kidney transplant.
To keep your risk of alcohol-related harm low, the NHS recommends:
- not regularly drinking more than 14 units of alcohol a week
- spread your drinking over 3 days or more if you drink as much as 14 units a week
- it's a good idea to have several alcohol-free days each week
Alcohol is also high in calories, so you'll gain weight if you drink regularly. Being overweight will also increase your blood pressure.
You should also avoid taking any illegal drugs after a kidney transplant, as they can damage your kidneys, cause a sudden rise in blood pressure and react unpredictably with your immunosuppressant medicines.
Finally, always check with your care team before taking any medicine, including medicine you get from a pharmacy and herbal remedies such as St John's wort. Some medicines could be potentially harmful if you have had a kidney transplant and are taking immunosuppressant medicine.
Immunosuppressants and infection
If you have a kidney transplant, you'll usually need to take immunosuppressant medicines for the rest of your life to prevent your body's immune system from attacking the new kidney.
Widely used immunosuppressants include tacrolimus, ciclosporin, sirolimus, azathioprine, mycophenolate and prednisolone.
However, taking immunosuppressive medicines on a long-term basis will weaken your immune system and make you more vulnerable to infections, so you'll need to take extra precautions against infection.
You should:
- avoid contact with people you know currently have infections, such as chickenpox or flu
- practise good personal hygiene – wash your hands regularly with soap and hot water, particularly after going to the toilet and before preparing food and eating meals.
- If you cut or graze your skin, clean the area thoroughly with warm water, dry it, then cover it with a sterile dressing.
You should also make sure your vaccinations are up to date, although you will not be able to have any vaccines that contain live viruses, such as the measles, mumps and rubella (MMR) vaccine.
When to get medical advice
The most common issues after a transplant are infection, rejection or the transplanted kidney not working properly.
Contact your transplant team, a GP or NHS 111 if you experience any of the following:
- a high temperature
- feeling hot and shivery
- headache
- aching muscles
- diarrhoea
- vomiting
- shortness of breath
- new chest pain
- fatigue or generally feeling unwell
- little or no pee
You may need prompt treatment to prevent serious complications from developing.
Risks
Although rates of serious complications have fallen sharply in the last few decades, kidney transplants – like any other type of surgery – are not risk free.
The risks of a kidney transplant include:
- risks related to the procedure itself
- risks related to the use of immunosuppressant medicines (which reduce the activity of your immune system)
- risks related to something going wrong with the transplanted kidney
Most complications occur in the first few months after a transplant, but can develop after many years.
Short-term complications:
Infection
Minor infections, such as urinary tract infections (UTIs), colds and flu, are common after kidney transplants.
You can also get more serious infections, such as pneumonia and cytomegalovirus (CMV), which may require treatment in hospital.
Blood clots
Blood clots can develop in the arteries that have been connected to the donated kidney. This is estimated to occur in around 1 in every 50 kidney transplants.
It may be possible to dissolve the blood clots using medicine, but it's often necessary to remove the donated kidney if the blood supply is blocked.
There is also a risk of developing blood clots in the legs. This is called deep vein thrombosis (DVT).
Narrowing of an artery
Narrowing of the artery connected to the donated kidney, known as arterial stenosis, can sometimes occur after a kidney transplant. Sometimes, it can develop months, or even years, after the transplant.
Arterial stenosis can cause a rise in blood pressure. The artery often needs to be stretched to widen it, and a small metal tube called a stent may be placed inside the affected artery to stop it narrowing again.
Blocked ureter
The ureter (the tube that carries pee from the kidney to the bladder) can become blocked after a kidney transplant. It can be blocked soon after the transplant - by blood clots, for example. It can also be blocked months or even years later, usually due to scar tissue.
It may be possible to unblock the ureter by draining it with a small tube called a catheter. Sometimes surgery may be required to unblock the ureter.
Urine leakage
Occasionally, pee may leak from where the ureter joins the bladder after surgery. This usually happens during the first month after the procedure. The fluid may build up in the tummy or leak through the surgical incision.
If you develop a urine leak, you'll usually need to have further surgery to repair it.
Acute rejection
Acute rejection means the immune system suddenly begins to attack the donated kidney because it recognises it as foreign tissue.
Despite the use of immunosuppressants, acute rejection is a common complication in the first year after a transplant, affecting up to 1 in 3 people.
In many cases, acute rejection does not cause noticeable symptoms, and is only detected by a blood test.
Acute rejection can often be successfully treated with a short course of more powerful immunosuppressants.
Long-term complications:
Immunosuppressant side effects
Immunosuppressants prevent your body's immune system from attacking the new kidney, which would cause the transplanted kidney to be rejected.
A combination of 2 or 3 different immunosuppressants is usually taken long term.
These can cause a wide range of side effects, including:
- an increased risk of infections
- an increased risk of diabetes
- high blood pressure
- weight gain
- abdominal pain
- diarrhoea
- extra hair growth or hair loss
- swollen gums
- bruising or bleeding more easily
- thinning of the bones
- acne
- mood swings
- an increased risk of certain types of cancer, particularly skin cancer
The doctor in charge of your care will be trying to find the right dose that is high enough to 'dampen' the immune system sufficiently to stop rejection, but low enough that you experience very few or no side effects.
Finding the optimal dose to achieve both goals is often a difficult balancing act. It may take several months to find the most effective dose that causes the least amount of side effects.
Side effects should improve once the right dosage is identified. Even if your side effects become troublesome, never suddenly stop taking your medicine because your kidney could be rejected. Speak to your GP or transplant team for advice.
Diabetes
Diabetes is a common complication of having a kidney transplant.
Diabetes is a lifelong condition that causes a person's blood sugar level to become too high. Some people develop it after a kidney transplant because, as they no longer feel unwell, they eat more and gain too much weight. Some types of immunosuppressants can also make you more likely to develop diabetes.
Symptoms of diabetes include:
- feeling very thirsty
- going to the toilet to urinate a lot, especially at night
- tiredness
Diabetes can often be controlled using a combination of lifestyle changes, such as changes to your diet, and medicine.
Read more about treating diabetes.
High blood pressure
High blood pressure is also a common long-term complication of a kidney transplant.
Many people who need a kidney transplant already have an increased risk of developing high blood pressure, and taking immunosuppressants can make the condition worse.
High blood pressure does not usually cause any noticeable symptoms, but it can increase your risk of developing other serious conditions, such as heart disease, heart attacks and strokes.
Because of the risk of high blood pressure, you will have your blood pressure checked at your follow-up appointments. You can also check your own blood pressure at home with a simple device available from most pharmacies.
Read more about testing your blood pressure.
Cancer
The long-term use of immunosuppressants also increases your risk of developing some types of cancer, particularly types of cancer known to be caused by viruses (as you will be more vulnerable to the effects of infection).
These include:
You can reduce your risk of skin cancer by avoiding exposure to the sun during the hottest part of the day and by applying complete sun cream to your lips and all exposed areas of your skin every day.
Your care team can give advice on your individual risks, whether you need regular check-ups, and any early signs to look out for.
The information on this page has been adapted by NHS Wales from original content supplied by  NHS website nhs.uk
NHS website nhs.uk
Last Updated:
16/12/2022 14:32:31