Overview
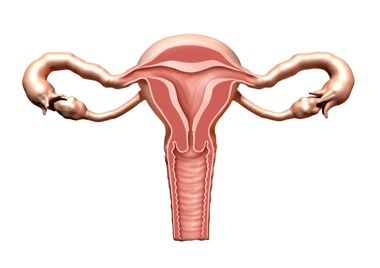
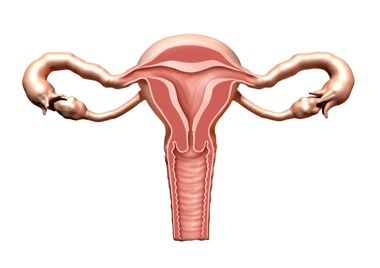
Fibroids are non-cancerous growths that develop in or around the womb (uterus).
The growths are made up of muscle and fibrous tissue, and vary in size. They're sometimes known as uterine myomas or leiomyomas.
Many women are unaware they have fibroids because they do not have any symptoms.
Women who do have symptoms (around 1 in 3) may experience:
In rare cases, further complications caused by fibroids can affect pregnancy or cause infertility.
Seeing a GP
As fibroids do not often cause symptoms, they're sometimes diagnosed by chance during a routine gynaecological examination, test or scan.
However, see your GP if you have persistent symptoms of fibroids so they can investigate possible causes.
If your GP thinks you may have fibroids, they'll usually refer you for an ultrasound scan to confirm the diagnosis.
Why fibroids develop
The exact cause of fibroids is unknown, but they have been linked to the hormone oestrogen.
Oestrogen is the female reproductive hormone produced by the ovaries (the female reproductive organs).
Fibroids usually develop during a woman's reproductive years (from around the age of 16 to 50) when oestrogen levels are at their highest.
They tend to shrink when oestrogen levels are low, such as after the menopause when a woman's monthly period stops.
Who gets fibroids?
Fibroids are common, with around 2 in 3 women developing them at some point in their life. They most often occur in women aged 30 to 50.
Fibroids are thought to develop more frequently in women of African-Caribbean origin.
It's also thought they occur more often in overweight or obese women because being overweight increases the level of oestrogen in the body.
Women who have had children have a lower risk of developing fibroids, and the risk decreases further the more children you have.
Types of fibroids
Fibroids can grow anywhere in the womb and vary in size considerably. Some can be the size of a pea, whereas others can be the size of a melon.
The main types of fibroids are:
- Intramural fibroids – the most common type of fibroid, which develop in the muscle wall of the womb
- Subserosal fibroids – fibroids that develop outside the wall of the womb into the pelvis and can become very large
- Submucosal fibroids – fibroids that develop in the muscle layer beneath the womb's inner lining and grow into the cavity of the womb
In some cases, subserosal or submucosal fibroids are attached to the womb with a narrow stalk of tissue. These are known as pedunculated fibroids.
Treating fibroids
Fibroids do not need to be treated if they are not causing symptoms. After the menopause they'll often shrink without treatment.
If you do have symptoms caused by fibroids, medicine to help relieve the symptoms will usually be recommended first.
There are also medications available to help shrink fibroids. If these prove ineffective, surgery or other less invasive procedures may be recommended.
Treatment
Treatment may not be necessary if you have fibroids but do not have any symptoms, or if you only have minor symptoms that aren't significantly affecting your everyday activities.
Fibroids often shrink after the menopause, and your symptoms will usually either ease or disappear completely.
If you have fibroids that need treatment, your GP may recommend medication to help relieve your symptoms.
But you may need to see a gynaecologist (a specialist in the female reproductive system) for further medication or surgery if these are ineffective.
See a GP to discuss the best treatment plan for you.
Medicine for symptoms
Medicines are available that can be used to reduce heavy periods, but they can be less effective the larger your fibroids are.
These medicines are described below.
Levonorgestrel intrauterine system (LNG-IUS)
The levonorgestrel intrauterine system (LNG-IUS) is a small, plastic T-shaped device placed in your womb that slowly releases the progestogen hormone levonorgestrel.
It stops your womb lining growing quickly, so it's thinner and your bleeding becomes lighter.
Side effects associated with LNG-IUS include:
LNG-IUS also acts as a contraceptive, but does not affect your chances of getting pregnant after you stop using it.
Tranexamic acid
If LNG-IUS is unsuitable (for example, if contraception isn't desired) tranexamic acid tablets may be considered.
They work by helping your blood to clot, reducing blood loss.
Tranexamic acid tablets are taken 3 or 4 times a day during your period for up to 4 days.
Tranexamic acid tablets are not a form of contraception and will not affect your chances of becoming pregnant.
Feeling sick, being sick or diarrhoea are possible side effects of tranexamic acid tablets.
Anti-inflammatory medicines
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and mefenamic acid, can be taken 3 times a day from the first day of your period until bleeding stops or reduces to manageable levels.
NSAIDs work by reducing your body's production of a hormone-like substance called prostaglandin, which is linked to heavy periods.
Anti-inflammatory medicines are also painkillers, but they are not a form of contraception.
Indigestion and diarrhoea are common side effects of NSAIDs.
The contraceptive pill
The contraceptive pill is a popular method of contraception that stops an egg being released from the ovaries to prevent pregnancy.
As well as making bleeding lighter, some contraceptive pills can help reduce period pain.
Your GP can provide you with further advice about contraception and the contraceptive pill.
Oral progestogen
Oral progestogen is synthetic (man-made) progesterone (one of the female sex hormones) that can help reduce heavy periods.
It's usually taken as a daily tablet from days 5 to 26 of your menstrual cycle, counting the first day of your period as day 1.
Oral progestogen works by preventing the womb lining growing quickly. It's not a form of contraception, but can reduce your chances of conceiving while you're taking it.
The side effects of oral progestogen can be unpleasant and include weight gain, breast tenderness and short-term acne.
Injected progestogen
Progestogen is also available as an injection to treat heavy periods. It works by preventing the lining of your womb growing quickly.
This form of progestogen can be injected once every 13 weeks for as long as treatment is required.
Common side effects of injected progestogen include:
- weight gain
- irregular bleeding
- absent periods
Injected progestogen also acts as a contraceptive. It does not prevent you becoming pregnant after you stop using it, although there may be a significant delay (up to 12 months) after you stop taking it before you're able to get pregnant.
Medicine to shrink fibroids
Gonadotropin releasing hormone analogues (GnRHas)
If you're still experiencing symptoms related to fibroids despite treatment with the above medications, your GP can refer you to a gynaecologist.
They may prescribe medication called gonadotropin releasing hormone analogues (GnRHas) to help shrink your fibroids.
GnRHas, such as goserelin acetate, are hormones given by injection. They work by affecting the pituitary gland, which stops the ovaries producing oestrogen.
The pituitary gland is a small, pea-sized gland located at the bottom of the brain. It controls a number of important hormone glands within the body.
GnRHas stop your menstrual cycle (period), but are not a form of contraception. They do not affect your chances of becoming pregnant after you stop using them.
If you're prescribed GnRHas, they can help ease heavy periods and any pressure you feel on your stomach. They also help improve symptoms of frequent urination and constipation.
GnRHas are sometimes also used to shrink fibroids prior to surgery to remove them.
GnRHas can cause a number of menopause-like side effects, including:
- hot flushes
- increased sweating
- muscle stiffness
- vaginal dryness
Sometimes a combination of GnRHas and low doses of hormone replacement therapy (HRT) may be recommended to prevent these side effects.
Osteoporosis (thinning of the bones) is an occasional side effect of taking GnRHas.
Your GP can give you more information about this, and may prescribe additional medication to minimise thinning of your bones.
GnRHas is only prescribed on a short-term basis (a maximum of 6 months at a time). Your fibroids may grow back to their original size after treatment is stopped.
You may be offered a type of GnRHas that also contains oestrogen and progestogen. It's taken as a tablet and can be taken for as long as you need it.
Ulipristal acetate
Ulipristal acetate (Esmya) is a medicine that can be used to treat fibroids. However, it should only be prescribed for occasional use if:
- you have moderate to severe symptoms
- you're an adult and you've not reached the menopause
- surgery and non--surgical procedures are not suitable or have not worked.
This is because there is a risk of serious liver damage and liver failure.
If your doctor thinks ulipristal acetate may be suitable for you, they should discuss the risks and benefits with you so you can make an informed decision.
If you decide to try ulipristal acetate, your liver function will be closely monitored using liver function tests before, during and after treatment.
Ask for an urgent GP appointment or call 111 if you develop symptoms of liver damage, such as:
- tummy pain
- yellowing of the skin or eyes (jaundice)
- dark pee
- tiredness
- loss of appetite
- nausea and vomiting
You may get these symptoms even after you stop taking ulipristal acetate.
There are currently no concerns with the emergency contraceptive pill ellaOne, which also contains ulipristal acetate.
Surgery
Surgery to remove your fibroids may be considered if your symptoms are particularly severe and medicine has been ineffective.
Several different procedures can be used to treat fibroids. A GP will refer you to a specialist, who'll discuss the options with you, including benefits and any associated risks.
The main surgical procedures used to treat fibroids are outlined below.
Hysterectomy
A hysterectomy is a surgical procedure to remove the womb. It's the most effective way of preventing fibroids coming back.
A hysterectomy may be recommended if you have large fibroids or severe bleeding and do not wish to have any more children.
There are a number of different ways a hysterectomy can be carried out, including through the vagina or through a number of small cuts (incisions) in your tummy (abdomen).
Depending on the technique used, a hysterectomy can be carried out using a spinal or epidural anaesthetic, where the lower parts of the body are numbed.
Sometimes a general anaesthetic may be used, where you'll be asleep during the procedure.
You'll usually need to stay in hospital for a few days after having a hysterectomy. It takes about 6 to 8 weeks to fully recover, during which time you should rest as much as possible.
Side effects of a hysterectomy can include early menopause and a low sex drive (loss of libido). This usually only occurs if the ovaries have been removed.
Myomectomy
A myomectomy is surgery to remove the fibroids from the wall of your womb. It may be considered as an alternative to a hysterectomy if you'd still like to have children.
But a myomectomy is not suitable for all types of fibroid. Your gynaecologist can tell you whether the procedure is suitable for you based on factors such as the size, number and position of your fibroids.
Depending on the size and position of your fibroids, a myomectomy may involve making either a number of small incisions in your tummy (keyhole surgery) or a single larger incision (open surgery).
Myomectomies are carried out under general anaesthetic and you'll usually need to stay in hospital for a few days afterwards. You'll be advised to rest for several weeks while you recover.
Myomectomies are usually an effective treatment for fibroids, although there's a chance the fibroids will grow back and further surgery will be needed.
Hysteroscopic resection of fibroids
A hysteroscopic resection of fibroids is a procedure where a thin telescope (hysteroscope) and small surgical instruments are used to remove fibroids.
The procedure can be used to remove fibroids from inside the womb (submucosal fibroids) and is suitable for women who want to have children in the future.
No incisions are needed because the hysteroscope is inserted through the vagina and into the womb through the entrance to the womb (cervix).
A number of insertions are needed to ensure as much fibroid tissue as possible is removed.
The procedure is often carried out under general anaesthetic, although local anaesthetic may be used instead. You can usually go home on the same day as the procedure.
After the procedure you may experience stomach cramps, but they should only last a few hours. There may also be a small amount of vaginal bleeding, which should stop within a few weeks.
Hysteroscopic morcellation of fibroids
Hysteroscopic morcellation of fibroids is a new procedure where a clinician who's received specialist training uses a hysteroscope and small surgical instruments to remove fibroids.
The hysteroscope is inserted into the womb through the cervix and a specially designed instrument called a morcellator is used to cut away and remove the fibroid tissue.
The procedure is carried out under a general or spinal anaesthetic. You'll usually be able to go home on the same day.
The main benefit of hysteroscopic morcellation compared with hysteroscopic resection is that the hysteroscope is only inserted once, rather than a number of times, reducing the risk of injury to the womb.
The procedure may be an option in cases where there are serious complications.
Read the National Institute for Health and Care Excellence (NICE) guidance about hysteroscopic morcellation of uterine fibroids.
Non-surgical procedures
As well as traditional surgical techniques to treat fibroids, non-surgical treatments are also available.
Uterine artery embolisation (UAE)
Uterine artery embolisation (UAE) is an alternative procedure to a hysterectomy or myomectomy for treating fibroids. It may be recommended for women with large fibroids.
UAE is carried out by a radiologist, a specialist doctor who interprets X-rays and scans. It involves blocking the blood vessels that supply the fibroids, causing them to shrink.
During the procedure, a special solution is injected through a small tube (catheter), which is guided by X-ray through a blood vessel in your leg.
It's carried out under local anaesthetic, so you'll be awake but the area being treated will be numbed.
You'll usually need to stay in hospital a day or 2 after having UAE. When you leave hospital, you'll be advised to rest for 1 to 2 weeks.
Although it's possible to have a successful pregnancy after having UAE, the overall effects of the procedure on fertility and pregnancy are uncertain.
It should therefore only be carried out after you have discussed the potential risks, benefits and uncertainties with your doctor.
Endometrial ablation
Endometrial ablation is a relatively minor procedure that involves removing the lining of the womb.
It's mainly used to reduce heavy bleeding in women without fibroids, but it can also be used to treat small fibroids in the womb lining.
The affected womb lining can be removed in a number of ways – for example, by using laser energy, a heated wire loop, or hot fluid in a balloon.
The procedure can be carried out either under local anaesthetic or general anaesthetic.
It's fairly quick to perform, taking around 20 minutes, and you can usually go home the same day.
You may experience some vaginal bleeding and tummy cramps for a few days afterwards, although some women have bloody discharge for 3 or 4 weeks.
Some women have reported experiencing more severe or prolonged pain after having endometrial ablation.
In this case, you should speak to your GP or a member of your hospital care team, who may be able to prescribe a stronger painkiller.
It may still be possible to get pregnant after having endometrial ablation, but the procedure is not recommended for women who want to have more children because the risk of serious problems, such as miscarriage, is high.
The Royal College of Obstetricians and Gynaecologists (RCOG) have more information about endometrial ablation.
MRI-guided procedures
There are also 2 relatively new techniques for treating fibroids that use MRI.
They are:
- MRI-guided percutaneous laser ablation
- MRI-guided transcutaneous focused ultrasound
These techniques use MRI to guide laser energy or ultrasound energy to destroy the fibroid.
These treatment methods cannot be used to treat all types of fibroids, and the long-term benefits and risks are unknown.
Research is still being carried out, but there's some evidence to suggest that these non-invasive procedures have short- to medium-term benefits when performed by an experienced clinician.
But the effects on pregnancy and women who want to have a baby in the future are not fully known, so this should be taken into consideration.
Find out more about:
Ultrasound-guided procedures
Transcervical ultrasound-guided radiofrequency ablation is a new procedure that uses heat to shrink fibroids.
Before the procedure you’ll be given a general or local anaesthetic, so you will not feel any pain.
A long, thin device that has an ultrasound probe at the end is passed into your vagina, through your cervix and into your womb.
The ultrasound probe sends images to a screen which helps your doctor see the fibroid. Heat is then applied to the fibroid to shrink it.
Because transcervical ultrasound-guided radiofrequency ablation is a new treatment, evidence about its safety and long-term effectiveness is limited.
Your doctor should explain the possible risks and benefits before you agree to have the procedure.